In my most recent blog on MIPS (read MIPS 101 here), I provided some background and basic concepts about the Merit-based Incentive Payment System that some PTs and OTs will be eligible to participate in beginning January 2019.
In this article, I will provide more detailed information about program eligibility and begin to explore options that you should consider for MIPS reporting.
Eligibility
All PTs and OTs who provide outpatient services for Medicare patients and bill under the Medicare Physician Fee Schedule (MPFS), and who meet certain volume thresholds discussed below, are eligible to participate in MIPS beginning in 2019. Organizations that provide services as an institution, such as Outpatient Rehabilitation Facilities (ORFs), Comprehensive Outpatient Rehabilitation Facilities (CORFs) and hospital outpatient departments billing Medicare as institutions are not subject to MIPS.
Low Threshold Requirements
CMS has established low threshold requirements for MIPS participation:
Eligibility |
Number of Patients |
Allowed Charges |
Service Volume |
|
Required Participation |
> 200 | > $90,000 | > 200 |
| Opt-In or Voluntarily Report |
Meet at least 1/3 of requirements above |
||
| Ineligible to Participate or Voluntarily Report | Do not meet any requirements above | ||
Most physical and occupational therapist Medicare providers do not meet all of the elements for required participation, but most meet the minimum requirements to opt in, based on service volume.
- If you meet all three low threshold requirements, you are therefore required to participate in MIPS in 2019. But, if you fail to report under MIPS (or a similar Quality Payment Program), you will receive a negative Medicare Physician Fee Schedule (PFS) adjustment in the payment year.
- If you are eligible to opt in and voluntarily report, you may receive a positive or negative payment adjustment. If you choose not to report, your Medicare PFS will remain frozen.
- If you are not eligible to participate, you will not receive a payment adjustment under MIPS.
Reporting Mechanisms for MIPS
As discussed earlier, the MIPS score for PTs and OTs is composed of only two components: Improvement Activities comprise 15% of the score and Quality Measures comprise 85% of the score. There are multiple methods for submitting MIPS Quality Measures data, including Claims, Qualified Registry, and Qualified Clinical Data Registry (QCDR) reporting.
In general, QCDR submission is most advantageous. It offers more clinical utility and relevance, ease and flexibility in reporting and outcomes measures that are higher valued in MIPS scoring.
A summary of common Quality Measure reporting mechanisms is summarized in the table below:
| Reporting Mechanism | Claims Based | Qualified Registry | QCDR |
| Available Quality Measures | Only measures approved by the National Quality Forum (NQF). | NQF measures, or measures already utilized in an approved QCDR. | May utilize NQF measures, or nominate new measures not already included in the NQF. |
| Group Size | Available for practices with 15 or fewer therapists | No group size limitation | No group size limitation |
| Clinical Utility | Low | Varies | High |
| Submission | Special procedure codes on claims forms | Registry organization | Registry organization |
| Types of Measures Supported | Primarily lower valued process measures | Process, patient experience, or outcomes measures | Process, patient experience, or outcomes measures |
| Relative Value | Lower value | Varies | Generally Higher value |
| Complexity | High | Varies | Varies |
| Acceptable Exclusions | Very specific and complex | Broad, includes clinical judgment | Broad, includes clinical judgment |
Quality Measure Submission
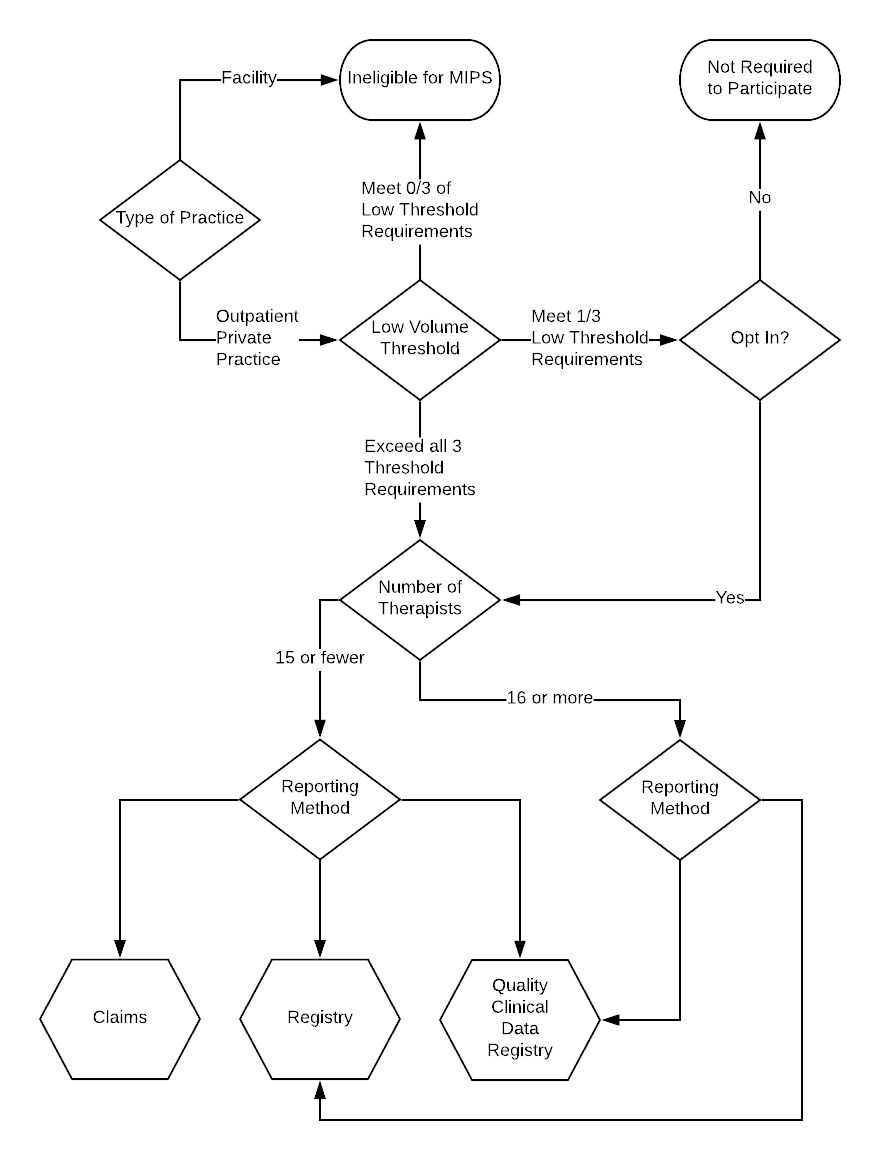
To help you decide what quality measure submission methodology to use, please refer to this decision tree.
- If you are submitting Medicare claims as a facility, you are not eligible for MIPS.
- If you meet all three of the low threshold factors described above, you are required to participate.
- If you meet 1/3 of the low threshold requirements, you may opt-in.
- If your group has 15 or fewer therapists, you may elect to submit MIPS Quality Measures via claims, registry, or QCDR.
- If your group has 16 or more therapists, you may submit MIPS Quality Measures via a registry or a QCDR.
Preparing for MIPS
As stated earlier, MIPS is a very complex and important program. But, it presents an immense opportunity for those who prepare to participate successfully. As a first step, we recommend familiarizing yourself with MIPS by reviewing the Quality Measures section of the CMS Quality Payment Program website. Additionally, we have developed a MIPS resource center to keep you up to date on MIPS. Learn more about participation thresholds, incentives, quality measures and more.
Coming: Scoring Details, Preparing for MIPS
In future articles, we will present more detailed information to help you successfully participate in MIPS. Specifically, we will discuss scoring in the Quality Measures component of the MIPS score, along with details about the financial implications.
Don’t miss our upcoming webinar with me on October 18th, 2018 to dive deeper into the practical implications of MIPS. Spots are filling fast so claim your seat today. Register here!
Disclaimer: The information provided herein is intended to be general in nature. It is not offered as legal or insurance related advice, and is not a complete description, or meant, or intended, to replace or be interpreted as specific, of Medicare requirements. Although every effort has been made to ensure the content herein is correct, we assume no responsibility for its accuracy. Contact Department of Health & Human Services (DHHS) Centers for Medicare and Medicaid (CMS) Services for more information.

Comments