What PTs, OTs, and SLPs need to know about this Medicare timed-services coding requirement.
Many procedures for rehabilitation therapists are billed in 15-minute units, using timed Common Procedure Terminology (CPT) codes that are created and copyrighted by the American Medical Association (AMA). The guidelines for aggregating timed procedure codes from the AMA and the Center for Medicare and Medicaid Services (CMS) vary slightly.
AMA guidelines, which are accepted by most commercial and private payers, always allow for an additional unit of service for each code when at least 8 minutes of service has been provided to a patient for that code. CMS guidelines, however, allow for a unit of service for every 15 minutes spent providing timed services for the entire visit, and rounded up to the nearest 8-minute increment.
Confused? You’re not alone.
This Medicare guideline, like many of CMS’s rules, is complex and unforgiving of mistakes. But in this guide, we provide a comprehensive overview of the 8-minute rule and how it affects Medicare billing for your outpatient rehab therapy practice.
What codes apply to the 8-minute rule?
CPT codes includes both time-based and service-based codes. You can bill service-based codes just once per session with a client, no matter how long the service takes to complete.
Examples of common service-based CPT codes include:
- PT evaluation (97161, 97162, 97163)
- PT re-evaluation (97164)
- Electrical stimulation (unattended) (97014)
- Hot/cold packs (97010)
- Group therapy (97150)
Time-based codes apply to services billed in 15-minute increments. Those increments are often included in the description of a CPT or HCPCS code, making it easy to identify them. Timed services require one-on-one, skilled therapy for the duration of the service, meaning that you cannot also document care or attend to another patient in the same timeframe. You must also be actively engaged with the patient, not simply supervising while he or she completes exercises or activities.
Examples of common time-based, rehabilitative therapy CPT codes include:
- Electrical stimulation (manual) (97032)
- Ultrasound (97035)
- Gait training (97116)
- Therapeutic exercise (97110)
- Manual therapy (97140)
- Neuromuscular re-education (97112)
- Self-care/home management training (97535)
- Prosthetic training (97761)
- Physical performance test or measurement (97750)
8-minute rule chart and how to calculate your units
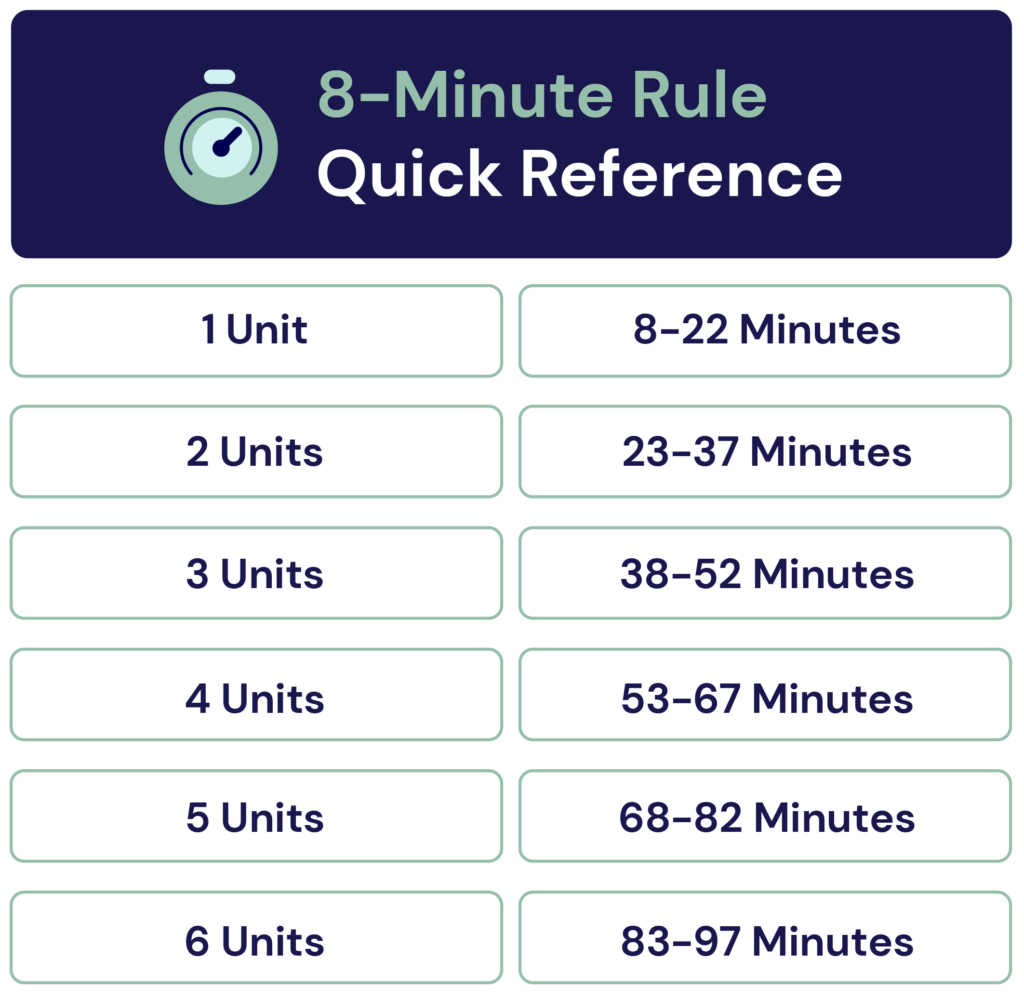
When determining how many units you can bill for a timed service, CMS requires at least 8 minutes of direct treatment for each billable unit. Furthermore, each unit occurs in 15-minute increments. Let’s break that down in our chart for a little more clarity:
After treating a patient, you can calculate your units using the following steps:
- Step 1: Add together all the time spent on providing timed services to determine how many units you can bill for in total.
- Step 2: Separate out each whole 15-minute units by CPT code. (Ex: 2 units of 97761 = 30 minutes of service.)
- Step 3: Here’s where things can get more complicated; if there are any remaining minutes that have not been converted into units, these are your “remainder minutes,” also known as “mixed remainders.” CMS allows billers to “borrow” and “round-up” other services to create whole units if there are enough remainder minutes.
Add whatever remainder minutes you have to any incomplete whole units. (Ex: 5 leftover minutes from 97110 can be added to 10 minutes of 97140, for a total of 15 minutes or 1 unit of 97140.) - Step 4: If there are still 8 remaining minutes left of a service, bill for another single unit. Since CMS allows 1 unit to be billed for any service that is at least 8 to 22 minutes long, the remaining 8 minutes qualify for CMS’s interpretation of the “8-minute rule.”
A little farther below, we have more examples to help illustrate these steps when calculating your units.
The AMA’s rule of eights
The American Medical Association (AMA) uses a slightly different system called the “Rule of Eights,” also known as the Midpoint Rule. Instead of adding the total session time for all time-based codes used, they consider each individual unit. You cannot bill for a unit unless the one-on-one treatment lasted at least 8 minutes.
For example, if you bill for 8 minutes of therapeutic exercise (97110) and 8 minutes for manual therapy (97140), you would bill two separate physical therapy billing units under the Rule of Eights (1 unit of 97110 on one line and 1 unit of 97140 on the second line).
Conversely, with CMS’s 8-minute rule, you would add both services to get a total of 16 minutes, then divide by 15 to get 1 unit billed. Based on the tie-breaker rule with CMS, you would choose one unit and only be able to bill for that service (97110 or 97140, not both).
Billing rules for the 8-minute rule
When Medicare reviews your claim, they will divide the total minutes for all timed services by 15. If the result of the equation leaves at least 8 minutes remaining before hitting another 15-minute increment, you can bill an extra unit. If there are less than 8 minutes, you cannot bill an extra unit.
As an example, a physical therapist provides 15 minutes of therapeutic exercise (97110), 8 minutes of therapeutic activities (97530), and 5 minutes of manual therapy (97140). All services are timed codes. Adding them together (15 + 8 + 5), the total time spent with the patient is 28 minutes.
15 + 8 + 5 = 28 minutes
28 / 15 = 1.86 (one unit, and a remainder)
28 – 15 = 13 minutes (the remainder)
15 minutes is the first unit, with 13 minutes remaining.
Answer: bill for 2 units total, 1 unit for 97110, and 1 unit for 97530
(97140 was only performed for 5 mins, so does not meet the 8-minute rule by itself)
In addition to the calculation rules, there are other Medicare rules that may also apply to billing under the 8-minute rule.
Appropriate billing modifiers
When submitting claims, it’s important to include any relevant modifiers that might impact the claim’s reimbursement. Here are some common modifiers for PT, OT, and SLP billing:
- CQ or CO: This modifier designates services performed in whole or in part by a physical or occupational therapy assistant (PTA uses CQ, OTA uses CO). According to CMS rules created in 2018, the modifier applies when a PTA or OTA provides at least 10% of the service. Services provided in tandem with the assistant and supervising PT or OT do not require the modifier.
- GA: This modifier indicates that the provider has an Advanced Beneficiary Notice (ABN) on file for noncoverage of a provided service that Medicare does not consider medically necessary or reasonable.
- GO: This modifier shows that an OT has provided services, usually in an inpatient or outpatient therapy setting.
- GN: This modifier shows that an SLP has provided services, usually in an inpatient or outpatient therapy setting.
- GP: This modifier shows that a PT has provided services, usually in an inpatient or outpatient therapy setting.
- KX: This modifier indicates that the client has exceeded the Medicare therapy threshold, but services remain medically necessary.
- XP: This modifier is used when a service is billed separately because it was performed by a separate provider.
- 22: This modifier is used for increased procedural services when the provider goes beyond what the code in question usually entails.
- 52: This modifier is used when the provider has reduced or eliminated the scope of a billed service at their discretion.
- 59: This modifier designates the billing of services that are not usually provided together, like NCCI edit pairs.
- 95: This modifier indicates services provided through telemedicine (live audio and/or video).
Billing with mixed remainders
The term “mixed remainders” refers to a situation in which your remaining minutes consist of more than one billing code.
For example, an occupational therapist performed 21 minutes of manual therapy (97140) and 17 minutes of gait training (97116) for a patient. After calculating the number of units, there are 2 remainder minutes of gait training and 6 remainder minutes of manual therapy left. In this case, since the total remainder is 8 minutes (combined), the therapist can bill for another unit. But which unit should the therapist choose?
Since there are more remaining minutes for manual therapy than gait training, the therapist will bill the final unit for manual therapy. If there were more minutes of gait training than manual therapy remaining, the therapist could have billed for gait training instead.
Billing for management, education, and assessment time
CPT definitions allow providers to include the time managing, assessing, and educating the patient about their condition as part of the definition of each code. When you use a time-based billing code, it comprises management and assessment time along with hands-on intervention and necessary supplies. Many outpatient rehab therapists lose billable time by failing to count these actions in their claims.
You can bill for assessment, management, and patient education activities as long as you provide these services on an individual face-to-face basis, including actions such as:
- Assessing before a time-based intervention
- Assessing intervention response
- Counseling and education about self-care for the patient to perform at home
- Responding to patient questions about the condition and intervention
- Documenting actions in the patient’s presence during the visit
Medicare 8-minute rule examples
Let’s look at some more examples to help illustrate how the 8-minute rule applies to billing for Medicare Part B.
Physical therapy example
A physical therapist spent 35 minutes performing therapeutic exercise (97110) with a patient along with 15 minutes of manual therapy (97140). In this case, the total billable time equals 50 minutes (35 + 15).
Divide 50 by 15 for a result of 3.3, leaving 5 remaining minutes. For this session, the therapist can only bill Medicare for 3 units since the remainder of 5 minutes is less than the 8-minute rule.
Occupational therapy example
An occupational therapist spent 27 minutes on prosthetic training (97761) with a patient who was recently fitted with the prosthetic leg. That visit also includes 11 minutes of self-care training (97535) with the device. In total, the therapist spent 38 minutes with the patient. Let’s break it down using the steps we outlined earlier:
- Step 1: Calculate the total allowed timed units. In this example, since the therapist spent 38 minutes of timed service, 3 units are allowed by CMS guidelines.
- Step 2: Calculate whole 15-minute units of service. 97761 is a complete unit in our example:
| CPT Code | Minutes | Full Units | Remainder Minutes |
|---|---|---|---|
| 97761 | 27 | 1 | 12 |
| 97535 | 11 | 0 | 11 |
- Step 3: Round up by adding together the remainder minutes. Here, you can “borrow” 3 remainder minutes of service from 97535 to round-up 97761 to bill 2 full units.
| CPT Code | Minutes | Full Units | Remainder Minutes |
|---|---|---|---|
| 97761 | 27 (+3 from 97535) | 2 | 0 |
| 97535 | 11 (-3 used by 97761) | 0 | 8 |
- Step 4: Allow one unit for any 8-minute remainders. In our example, there are still 8 minutes of 97535 available, so one additional unit of 97535 is allowed.
- Final answer: 2 units of 97761, 1 unit of 97535, for a total of 3 units.
Speech-language pathology example
A speech therapist* performs 35 minutes of therapeutic intervention of cognitive function (97129) with a patient who is recovering from a stroke. Before starting that therapy, however, they also conducted a cognitive performance test (96125) for 55 minutes. In total, the therapist spent 90 minutes with the patient, allowing for 6 units to be billed.
- 2 units of 97129, with 5 remaining minutes.
- 3 units of 96125, with 10 remaining minutes.
- 1 additional unit of 96126. Since there are 10 remainder minutes of 96125, a fourth unit of 96125 can be billed.
(*Note: According to ASHA and CMS, most SLP codes are untimed with a few exceptions. If you are unsure of if a code is timed or untimed, ASHA recommends noting which codes include a time frame in their description. Untimed codes will not have an associated time in their description.)
Frequently asked questions about the 8-minute rule
It’s easy to get confused by Medicare’s rules, and the 8-minute rule is no different. Here are some frequently asked questions about these rules and where you can find more information.
Is the 8-minute rule mandatory?
Using CMS’s interpretation of aggregating timed procedure codes (the 8-minute rule) is mandatory when you submit reimbursement claims for Medicare Part B billing.
However, some private insurers use the 8-minute rule, the AMA Rule of Eights, or their own proprietary billing rules. Review the rules for each insurance company carefully to avoid billing issues, denials, and delays.
Can you bill for documentation time?
While you cannot bill specifically for documentation completed after the patient visit, you can include documentation done during the visit when it occurs alongside other services.
For example, if a PT provides patient education during a session while also documenting the provided education, the full amount of time for these activities is billable. You cannot bill for the documentation minutes alone if documentation is done post-visit.
What happens if you have 3 units but not enough remainder units to bill for a full timed unit?
Let’s look at an example in which a physical therapist provides 42 minutes of therapy in total, including 30 minutes of therapeutic exercises, 7 minutes of therapeutic activities, and 5 minutes of manual therapy. They could bill 2 units for therapeutic exercise, but what about the remaining unit?
Since neither of the remaining codes have enough time for a full unit, the biller should combine them into one unit instead. They should bill one unit for therapeutic activities since it comprises the majority of the time (7 minutes compared to 5 minutes) when combined with the other code.
What happens if a therapy assistant helps with some portion of a timed service?
As described above and in our CO/CQ modifier guide, you use the CO code modifier for OT or CQ code modifier for PT when an OTA or PTA assists with time-based client services. If you provide services in tandem with the assistant, you do not use the code modifier. The modifier refers only to services provided independently by an OTA or PTA.
How can I best maintain compliance with Medicare?
In general, make sure to always supply documentation with timed billing codes that support direct, intense one-on-one time with the patient. Check the CPT code book and each payer’s rules to make sure you adhere to the definitions provided for the billed code and are using the appropriate version of the “8-minute rule” for each payer.
A single system for EMR and billing can also help immensely in maintaining Medicare and payer compliance. Clinicient’s Insight Platform is designed to simplify the complex, with a range of features including:
- Automatic unit calculations: Speed-up claim creation with simple, automatic CPT code selection and unit calculations based on the therapist-documented services provided.
- Customizable payer rules: Whether claims are going to Medicare, private, or commercial payers, or you’re using the Medicare or AMA version of the 8-minute rule, the Insight Platform offers customizable payer rules so you can reduce billing errors and simplify clinic compliance.
- Automatic Medicare updates: Never miss an important Medicare update, as our platform will automatically incorporate new rules, NCCI edits, or other compliance concerns before they go into effect.
- Financial reports, threshold alerts, and much more: Access financial reports for your clinic, plus other billing automations, like therapy threshold alerts, automatic charge capture, and so much more. Juggling the many rules of Medicare can be daunting, but with a single-system for EMR, billing, analytics, MIPS, and more, our expertise can be your clinic’s advantage.
Want to learn more about the Insight Platform? Schedule a free, no-obligations demo today.
Where can I find more information on Medicare’s 8-minute rule?
You can learn more information about Medicare’s 8-minute rule on the CMS website, or using the following PDFs:
Additionally, you can find more information specific to your specialty with the following organizations:


Comments